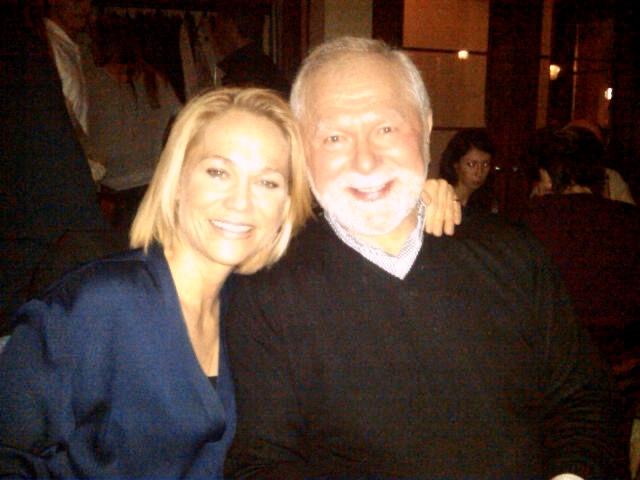
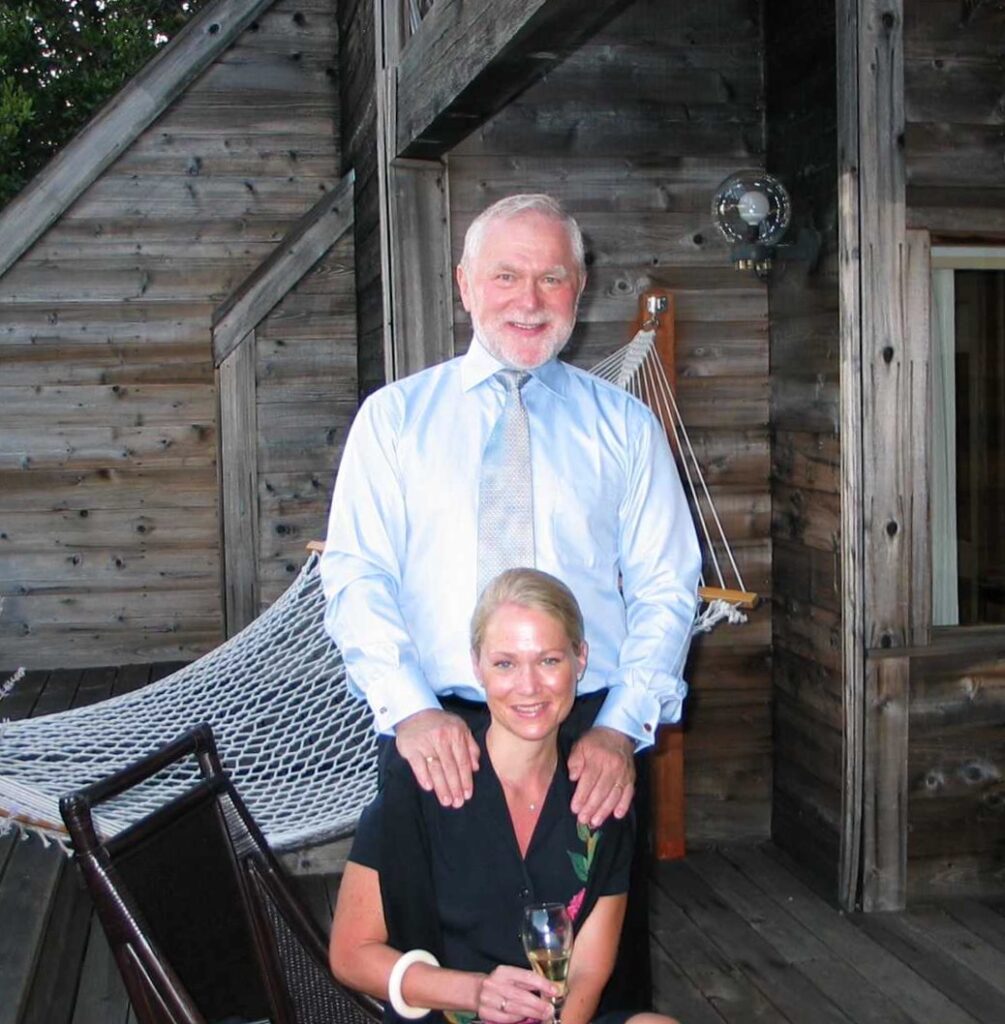
Written by Lisa and Michael Hehenberger
We have both donated a kidney to our sister / daughter Karin, in the years 2023 and 2009, respectively. Having donated and successfully recovered, we’d like to share our experience as well as proposing ways to increase the number of “live donors”, willing to help other patients in need.
Background
Karin has struggled for many years with the dire consequences of Type I diabetes. She was diagnosed before her 17th birthday and her diagnosis affected our family in significant ways. Karin and Lisa were very close growing up, playing together, traveling, playing tennis, and sharing an active family life. Little sister Anna, being 11 years younger than Karin (and 8 years younger than Lisa), was perhaps less affected, but still experienced that the mood had changed at home. Suddenly, Karin was no longer the person whose sisters and parents Ulla and Michael considered “invincible”. The diagnosis also coincided with a move to Paris where the family spent four years, from 1989 to 1993. Karin graduated from high school in Paris in 1991 and moved to Stockholm to study medicine. In 1993, Lisa joined her to study Economics. Karin & Lisa lived together and successfully earned their respective degrees. Karin’s goal was to get a deep understanding of the molecular mechanisms responsible for Type I Diabetes. She completed her MD Ph.D. at Karolinska, Stockholm. While her parents and little sister had moved to California, the two older sisters lived together in Sweden for a few years until they went their separate ways due to work, study, and eventually start their own families. Lisa got a Ph.D. in Venture Philanthropy and is now a Professor at ESADE, a Spanish business school. Karin & Lisa stayed connected and visited each other at least once a year although they lived in different countries, in the United States and Spain, respectively.

Karin’s Kidney Failure
In 2009, when Karin’s kidneys stopped functioning properly and she required dialysis or a transplant, her father Michael stepped up and volunteered to donate a kidney. Lisa was pregnant with her second child and living in Spain, but came over to New York to support the family for the surgery. Being pregnant, Lisa couldn’t be a donor but told Karin that if she ever needed a kidney again, she would be a candidate for another live donation.
Father Michael’s Donation in 2009
Being 63 years old, rigorous tests were needed to qualify father Michael for his kidney donation. As two complicated parallel surgeries are required, to extract a kidney and to transplant it into the recipient’s body, it is important to minimize all risks and to make sure the donor is healthy and that the kidney is in good enough shape to survive for many years in the recipient’s body. Two highly qualified surgeons have to team up to achieve this goal. Both patients recovered quickly. In fact, less than 2 months after his donation, father Michael participated in a hike to the Himalayan foothills at the border of India and Nepal, close to Darjeeling. As an avid runner, he measured his performance before and after his surgery: The decline in speed and endurance was about 9% about one month after surgery, not serious enough to give up his plan to see four of the world’s five highest peaks! He did the hike with four friends, all highly supportive. A highlight was his lighting of a candle in a Buddhist monastery. It was a memorable spiritual experience.
Sister Lisa’s Donation in 2023
While father Michael’s sole kidney was functioning very well, Karin’s transplanted kidney had suffered from the negative side effects caused by immunosuppressant drugs that have to be taken daily to avoid organ rejection. As a consequence, Karin was in need of a second transplant, 14 years after her first. Lisa donated a kidney to her sister in April 2023. In what follows she has tried to provide as much detail as possible so that others can understand what it felt like (although each experience will be different). Donating a kidney is not easy, but it is a unique and wonderful opportunity to save someone’s life – with relatively low risks for the donor. Lisa’s bond to her big sister has grown stronger through this shared experience, but also by the fact that Karin has a part of her sister inside her body. Donating a kidney is an act of love that generates more and stronger love. That is how Lisa feels.
Pre-Screening, Tests, Planning, and Surgery (as told by Lisa)
In 2022, Karin told me that her kidney values were alarmingly poor and that she had to start preparing for a new transplant. What I had once promised was suddenly a reality. I knew her health had deteriorated over the past years but I think I was too scared to start informing myself properly about the process. I decided to come over from Barcelona (where I live) to New York in the summer of 2022 to help Karin get through a hip replacement surgery and take care of Karin’s daughter Liv. It was also a good opportunity to undergo all the screening tests to become a donor.
At this time, I was put in touch with the kidney transplant team at Columbia Presbyterian Hospital in New York City. I was assigned a coordinator who took care of booking all my appointments and informing me of the general process. Apart from a number of blood tests, urine tests, a CT-scan, EKG and X-rays I also met with a psychiatrist, a financial advisor, a social worker, my surgeon and a nephrologist. All the tests and meetings took almost a week. It was a tiring experience but it felt important to be fully informed – and of course the hospital needed all the information about me to assess my suitability as a donor and the match with my sister. My children (then 15 and 12 years old) were worried for me and I wanted to feel confident that I could provide them with all the information they needed so that I could reassure them.
The first meetings were with the coordinator, social worker, financial advisor and psychiatrist. They asked a lot of questions about my motivation for donating a kidney, informed me about the risks and wanted to understand if I was mentally stable and fit to be a donor. They highlighted the potential health problems that could result from the surgery in the short term and from complications over time, as well as financial risks if I would lose income as a consequence. They wanted to make sure that no one had pressured me into becoming a donor. I was not fully prepared for all these negative aspects and I felt quite down after these meetings. The meetings with the surgeon and the nephrologist were much more positive. They explained how being a donor of course involves risks, but that most donors live long and healthy lives. They also explained how I was an ideal donor because of my healthy lifestyle, my health condition and my age (47). By the time you reach my age most people have developed habits and routines that normally are life-lasting. Seemingly healthy younger donors might still change and become smokers, alcoholics, etc. I felt more confident about the donation after these meetings. I also spoke to my dad about his experience and to another kidney donor who had donated her kidney to a stranger. I am in awe of people who decide to donate a kidney to someone they don’t know.
I also had an interesting conversation with a Jesuit priest who I consider to be a wise man and who has counseled me before. I told him about how I worried about my children. He said two things that stayed with me and were important in the process: He said that donating a kidney may involve risks but it is also an incredible opportunity to do good, to save my sister’s life. He also said that doing this act of kindness and generosity would be a wonderful example for my children. As a parent one tries to be a role model – by donating a kidney I could demonstrate my love for my sister and this could help bring my children closer together too. I think I was already convinced to go ahead with the donation, but this conversation and the subsequent reflection really changed my attitude towards the donation from sacrifice to gratitude.
A few weeks after the tests (in September 2022) we received the green light that the donation could proceed. We were a good match and I had fulfilled the necessary screening conditions. I would need to stay in the United States for a month for the procedure as I needed to be there at least a week before for additional tests and then at least two weeks after the surgery to heal and not to risk blood clots on the plane. Karin and I discussed potential timings considering her recovery from the hip replacement and my work schedule (I am a professor at a business school) and the children’s school holidays.
In February 2023, we finally were able to plan the transplant for April 2023. I had to prepare everything at home, cancel a class I was teaching and prepare the logistics at home so that the children would be well taken care of. I am divorced with full custody and my ex-husband agreed to be responsible for the children during my absence. Unfortunately, my son had surgery on his ankle in March so when I left him, he was still recovering from that.
I arrived in New York at the beginning of April and my sister was in very poor shape. She was admitted to hospital and had started dialysis. I wondered if we had waited too long. I had some additional blood and urine tests to do during the first few days. I caught a slight cold during those first days and it turned out to be COVID! I had avoided COVID during the pandemic so it felt like very unfortunate timing. My parents also got sick and we were confined in their house for a few days. We had to postpone the surgery another week to allow me to test negative. On the positive side, my sister was getting dialysis every other day and was starting to feel stronger.

When the date of the transplant finally arrived, we were all eager to put it behind us, but also worried. The psychiatrist had told me that I needed to separate the act of donating the kidney from the outcome (that the kidney would work for my sister). I found this difficult to do. My parents drove us to the hospital early in the morning and we were all nervous in anticipation of the event. I imagine that it must have been tough for my parents to send two of their (three) daughters off to surgery at the same time. At the hospital we registered and waited in the waiting hall. I was called first and went to the pre-operatory room with my dad. The nurses prepared me by taking my vitals and asking many questions. The surgeon and the anesthesiologists also stopped by to explain the procedure and prepare me. I then went to the operating room and I don’t remember anything else. I woke up about four hours later in the recovery room. The nurse told me that the first thing I said was: “Now I only have one kidney!”. As I was waking up, Dr. Mark Hardy who had founded the Columbia Presbyterian transplant unit, came to check on me. He told me that the kidney was already working for my sister – on the operating table! I was so happy I started crying and he cried too. It was a beautiful moment.

A few hours later I was sent up to my hospital room and my parents came to see me. I was tired but happy and did not experience pain yet. The day after was the worst – I had intense pain in my left shoulder and my stomach was bloated and full of gas. I felt terrible. It helped to start walking around and when they removed my catheter after 24 hours, I was more mobile. My sister and I were able to see each other and hang out. As we both felt better, we ended up having a positive bonding experience in hospital. The hospital staff was truly remarkable. The nurse team (especially nurse Annie) was very attentive and I felt totally cared for. I must admit I was a bit scared of leaving hospital and having to manage everything on my own. There was a comfort in the hospital routines and even the controlled food. When my dad picked me up from hospital on the third day I cried in the car and couldn’t stop crying when I came back to my parents’ house. Maybe it was just the relief that it was over.
Recovery Period
The surgery was laparoscopic meaning that the incision is small (just big enough to remove the kidney) with three other small incisions for the instruments they insert. They blow up your belly with gas so that they can operate without making a bigger cut. This means that it takes a while afterwards for all the gas to go away. It helps to walk around. I understood that the procedure also causes the lungs to compress which is why I found it difficult to breathe for at least a couple of weeks after the surgery. The shoulder pain was also due to the procedure. However, the advantage is that the surgical healing is faster.
After the surgery of course the donor feels much worse than before the surgery – while the transplant patient generally feels much better than before. Karin had a lot of energy and Lisa had very little. This may sound strange but makes sense since the donor has lost a kidney while the recipient has gained one. Walking a little more each day is very helpful. It helps to have a device that tracks your steps to keep your motivation going. Later, at home, the sisters had a pleasant recovery period at Karin’s house with her daughter Liv. It felt important to share the experience and to support each other. The sisters also received support from their parents. It helped to stay closely connected with family at home and speaking to them every day. Younger sister Anna also came to visit during the recovery, along with her baby boy Freddie. Supportive messages and calls from friends were helpful.

Once back home in Barcelona Lisa felt tired but also euphoric about the experience. She could walk around and felt like crying out of joy: Lisa felt grateful that everything went well and it somehow made her appreciate her loved ones and everything around her. Then it was tough to get back into a work routine as there was a pile of things to get on with, with somehow limited energy levels. In addition, the children also needed extra attention and care. The first two months went by in a haze and Lisa hardly had time to catch her breath. However, after two months, everything was starting to feel normal again. Lisa is back into her exercise routine. As her father, she measured her performance before and after the kidney donation: after a drop of about 10%, it took her 9 months to get back to her pre-op fitness level. Her renal parameters are also coming back to levels almost as strong as before.


Final Words About Kidney Donations
Donating a kidney is a big decision, but ultimately an incredibly positive experience. Both Michael and Lisa felt good about their donations. They have recovered nicely and do not experience a diminished quality of life. By sharing their respective stories, they hope that their experience will be helpful for others who are considering a donation. Donating a kidney to a family member should not be a very difficult decision: the Pros dominate the Cons.
Donating a kidney altruistically, to a stranger, is a much bigger deal. We believe that society should consider some kind of compensation for such an act, to increase the number of live donors. There are important ethical arguments that are made in such situations, but the benefits for society should outweigh arguments against. If financial compensations are unacceptable, there may be other ways to reward donors, perhaps by means of free healthcare benefits and free life insurance. Since survival rates are statistically unchanged after donation of a kidney, a free life insurance as guaranteed by government should not be an extra burden to other tax payers. Still, it would reassure donors.
As to deceased donors, Spain seems to have created a system that should be emulated by other countries. Kidneys received from live donors will be generally healthier and have a better chance to last a long time, but, compared to dialysis, organs from deceased donors are still a better choice.

As Easter passes, I reflect upon the concept of rebirth, as fantastic as it may seem, but today of all days it seems possible.
Is organ transplantation rebirth, a do-over, or is it simply the continuation of many years of battling chronic kidney disease with a degree of improvement?
The moment of the transplant, when the kidney starts working inside the body of the recipient, is nothing less than a miracle, only comparable to birth in medical terms. Based on my experience with three transplants, that euphoria continues for a time period after the procedure where gratitude and happiness are dominant while fear for the future is suppressed.
The recipient and the donor recover together in many cases, as it was in two of mine (father and sister) and create a bond stronger than they had before. That bond of course also includes complex feelings of fear for the donor’s future health, and fear of messing up the gifted kidney.
Over time, the new kidney settles in, and much of what the recipient could not do before is possible. In my case, I was able to work full time, travel, do sports, eat and drink freely and be happy since I was not so tired or in pain anymore.
However, over the long term, due to the lack of new and better immune suppressants to preserve the organ safely, the side effects and the complications become more serious and impact life in a major way. Headaches, tremors, hypertension, diabetes, gastrointestinal issues, infections, cancers, mental health problems such as anxiety and depression, as well as the decline of kidney function lead back to the situation prior to the transplant.
I have no illusions of living forever and even less of living without pain or suffering. It is part of life’s cycle to start healthy and new, and end old and broken.
All I am seeking is a little longer to enjoy the freedom and happiness. I savor the time before I have to go back to that broken state from where I was saved – not just once but twice.
Thank you Pappa and Lisa. And thank you to the family who decided to donate their daughter’s pancreas to me.



I had my first kidney transplant on March 12, 2009, and from all perspectives, it was a great success!
It allowed me to go on to have a pancreas transplant (without a normal kidney function, it would have been hard to go through that very tough surgery), venture out to start a company (Lyfebulb), and conceive a child. Those were the highlights.
But let us not forget everything else that this kidney allowed me to do. First of all, it let me live. Without it, I would most likely have been on dialysis within a year or so, and the life expectancy of a diabetic person on dialysis is less than 5 years. I also traveled to many interesting places, got married, enjoyed new and old friendships, and participated in sports such as tennis and running during these 14 years.
So, to start, I want to thank my donor, my Father, for this life-saving gift.
However, for the past 3 years or so, my kidney has been in steady decline. Likely, some combination of Covid, the stress of the breakdown of my marriage, leaving Manhattan and setting up my life in an old but beautiful house in Westport, CT, balancing the roles of an entrepreneur and single mother, and the effects of the drugs that suppress my immune systems were all contributing factors. Most importantly, the fibrosis caused by tacrolimus truly put my kidney through the wringer. It is so sad that the very drug that is the gold standard for transplant patients (to avoid rejection) is also the one that causes decline of kidney function over time.
Over the past year, I started noticing a few things about my health that were troublesome. First, I was more tired and less social than before. I just didn’t have the energy to embrace situations I craved in the past. Luckily, my daughter is only 5, so she goes to bed early, and that allowed me to go to bed early as well. Importantly, I did not ever let this fatigue affect my attitude at work or the care taking of my daughter. But it did affect my health.
I was also much more sensitive to feeling cold. The only times I was really comfortable were in direct sunlight (which causes skin cancer in people like me) or in my sauna. I would sit in my sauna several times a day just to feel better. It did not do wonders for my iPhone’s performance when I brought it in with me.
It was painful to be this cold and it was due to my grave anemia, which was driven by kidney failure. Despite treatment with erythropoietin stimulating drugs, such as Aranesp, and even a blood transfusion, my hemoglobin would hover around 6-7 (versus a normal range of X – Y). Anemia also impacted my ability to do exercise, since my muscles would not get enough oxygen to function, and even my heart was struggling at high exercise levels.
During this year, I also went through several surgeries for my skin cancer, including one on the tip of my nose, which needed flap reconstruction by a plastic surgeon. He remarked afterwards that my clotting time was quite long. I explained that both my platelets were low and those I had were faulty, due to my low kidney function.
My family noticed my decline as well, and during the summer of 2022, my father asked me to speak to my middle sister, Lisa, who previously had offered to give me one of her kidneys (without me asking). As I was just 40 at my initial transplant, it had always been the plan that my father was to give me the first kidney, and then one of my sisters would give the second.
Lisa has always been of excellent health. She is 5’11’ and runs almost daily, has a resting pulse of 50, and is also an incredibly loyal and lovely person. Her children are 16 and 13 years old, so she was past the physically demanding baby years. I set up a zoom call with her, since I didn’t want to talk to her without seeing her. She immediately said, “I already told you I was going to give you a kidney”. It was such a relief for me that I didn’t even have to ask her.
I have heard stories from other people. Some people worry about that question so much that they avoid family gatherings and getting close to friends.
Now it was a question of when and how to coordinate some important events ahead of time. I needed to have a total hip replacement in August of 2022, and we were discussing whether it made sense to do the transplant before or after that, since that surgery would put additional stress on my kidney. I ended up getting the hip done successfully, but the stress of the surgery caused an additional drop in hemoglobin. So I needed a blood transfusion that September. This procedure gave me the “boost” to make it through the Fall.
Before that surgery and the corresponding impact, my nephrologist had wanted to wait to do the next transplant until my function had declined further. But I was feeling weaker and weaker, so over Christmas, we agreed to do the transplant over Easter, in April of 2023.
My sister Lisa works as a professor at a business school in Barcelona, Spain, and she needed to plan for a month of absence and also of course for childcare during the time she was going to be away.
We both got extensively evaluated from August of 2022, first with respect to matching our blood types, and then our tissue types, and finally making sure I didn’t have antibodies toward her. Our general health, mental health and social and financial support were evaluated as well, and I especially needed to be assessed from a cancer and infection perspective. I also needed to be up to date with respect to vaccinations and dental care as well as any cancer screenings.
Lisa was strong and passed with flying colors. While I had a nuclear stress test that flagged for potential heart blockage. The surgery required for a kidney transplant is serious and cardiovascular clearance is a critical part of evaluation. Since the stress test was abnormal, they required I undergo an angiogram, which involved using a contrast agent. I was very worried about this, since contrast is toxic to the kidney and I was convinced that the stress test was erroneous (I had always had a healthy heart). However, based on the upcoming surgery, and my many years with diabetes, they would not let me avoid the angiogram.
The day of the angiogram I was so nervous. I knew there was a huge risk involved here, since my kidney function was already only 12 percent, and I could not really go lower without extensive problems. My dad took me to the hospital and the procedure ended up showing no blockage; the stress test indeed was indeed erroneous.
However, the effects of the procedure kicked in. The sedation caused massive nausea in me. I could not stop vomiting for the next 24 hours. I tried to treat this at home, but could not keep anything down, and I had to go back to the emergency room the following day to get IV fluids and IV anti-emetics.
The interventions worked on my nausea, but the damage to the kidney was extensive. Between the contrast and the dehydration due to the vomiting, my poor kidney was in acute failure. Within a week I was in hypertensive crisis and severe uremia. My kidney function crashed to 5 percent. Dialysis was the only option for me to survive.
The symptoms I had experienced for the past year seemed like heaven compared to how I was feeling at that time. My head was pounding, I was severely nauseous, and my legs did not fit into any of my pants. My ankles were bloated and my face was unrecognizable. I was severely tired and depressed. I was hospitalized and emergency dialyzed for four days after getting a catheter into my neck vein to link to the dialysis machine that would save my life.
I have never in my life felt as bad as I did in the days before the dialysis. Although it saved my life, the sessions (9 in total, over three weeks) were pure misery.
Two things saved me: thinking about my daughter, and knowing I had to get well for her, and the transplant scheduled for April 13. I knew this was a phase that would endure, and once the transplant worked, I would feel much better again.
Writing about my experiences helped to keep me on track. I have always loved writing and it helped me keep my thoughts from spinning out of control.
My support system kicked in. My sister traveled to NY and came to visit me when I was in the hospital getting dialyzed. My friend and colleague, Leslie, brought food and amazing sweatpants to cheer me up. My family back in Westport were close in touch and took excellent care of my daughter. I truly discovered what a wonderful support system I have, from the mothers of my daughter’s friends to my amazing mother and father.
And we got dealt one more ringer. Shortly after her arrival for Easter weekend and final, routine pre-transplant donor tests, my sister was diagnosed with Covid! And she passed the virus to my parents. None of them had had covid for the past three years, but now they got it! I lost my family network of support for a week, while I was at my weakest.
I had originally been scheduled to do just three outpatient dialysis sessions after being released from the hospital. Now, I was worried about the timing of the surgery, which was deferred until a week later. I needed more outpatient dialysis (6 versus 3 sessions) to make it to the transplant. No one could stay with my daughter and me. My parents used masks and drove me to my dialysis and my daughter to school, and our nanny was very helpful in her support.
Ultimately, the surgery was moved to April 19, and I was as ready as I could be!!
Continue reading part 2 of Karin’s journey: The Dialysis Cleanse



Since studying diabetes in medical school, I have been awfully afraid of kidney disease. The complications of diabetes both scare and fascinate me – so much that I went on and did a PhD in diabetic complications followed by a post doc at Harvard studying the same. I had an almost obsessive fascination with the issues I might face in the future, if I were unlucky.
25 years later I am on dialysis – the ultimate, final step in kidney failure treatment. Dialysis implies the kidneys are no longer working, even minimally, and a machine needs to take over the very important functions normally executed by those bean (or as my daughter has come to name them “croissant”) – shaped organs.
The kidneys do more than excrete urine. In fact, many of the functions are not well known to most, including their importance in blood pressure regulation, hemoglobin production (which carries oxygen to all tissues), calcium and phosphate metabolism and electrolyte regulation. However, what most of us know is that kidneys filter out toxins and break down certain drugs and compounds. That means that if the kidneys don’t work well, you literally become toxic (uremic) and those compounds that are meant to be broken down in the kidneys remain at very high levels in the blood.
I was facing dialysis in April of 2023, due to a few unfortunate events that can be seen as cautionary (and, by me, as detrimental). I had been planning my second kidney transplant for a while. I had lots of time to speak to my donor (my sister), get used to the idea of going through surgery again and plan for the recovery carefully. However, during my cardiac evaluation, an errant stress test triggered a confirmatory angiogram, which luckily was negative for blockage. But this test (angiogram) used a contrast agent which led to my kidney failing rapidly and acutely.
I started feeling very differently than before. My chronic fatigue that I was getting used to was worse. My sensitivity to cold was complemented by nausea, itching, persistent high blood pressure (sky-high levels), followed by headache and blurred vision. I was uremic and so swollen that my clothes did not fit, and I was very uncomfortable.
I had to be emergency-hospitalized, and right before my first dialysis session, I was more scared than I have been of anything in my life.
I had pictured the scenario many times, a machine taking over from my kidneys, vacuuming my blood out, filtering and cleaning it, then pushing it back into my vessels. I envisioned myself hooked to a machine, without which I would slowly die of internal poisoning.
The reality was that my first session was in a low-lit room at Columbia Presbyterian hospital, in a comfortable bed, with a Samsung screen in front of me, and a gentle nurse who took me through the process. Three hours later, I was rolled back to my room. It was not that bad!
I went through another two sessions in the hospital, one a day, which is very aggressive, but my toxicity levels were bad and I needed detoxification desperately to get ready for my transplant.
When I was released, I had to go to dialysis in an out-patient setting, and the scenario was very different.
I was now taken to a brightly lit, huge hangar-like room, with multiple chairs seated close by each other. I heard beeping sounds constantly and had very sick patients on either side of me. The personnel were friendly and one nurse offered me a fleece blanket, headphones and a few documents to read in my own time, and then she hooked me up to the machine.
The beeping drove me crazy, so I placed the brittle, plastic headphones over my ears (they barely covered the ear). The chair was one of those recliners that if you move the least, the whole thing goes horizontal; there is no middle step. And the blanket was flimsy, but appreciated. It definitely made me less cold since the environment gave me chills. During my first session, an elderly woman kept crying out “help me” every five minutes, until an ambulance came to pick her up. Next to me was an older man who had issues breathing. I tried to shut my eyes.
When I was done, three hours later, the nurse asked me to weigh myself again (a large scale sits at the entrance) to make sure enough fluid had been “taken off”. I felt wobbly and had a headache that was explained by the “electrolyte shift” that had taken place.
I bravely walked out to be driven home by my mother. I thought about those without family who had to go home by themselves after these sessions. The physical and mental trauma that had taken place do not set one up well up for cooking dinner, or driving a car.
That evening, I was truly exhausted. But the next day, I felt remarkably better! I enjoyed a healthy meal for the first time in quite a while without nausea, could go for a walk without fatigue and generally felt “cleaner”.
Dialysis is, for sure, not worse than death, which is what I had compared it to previously. But I reflect, surely there must be a way to improve the way the treatment is being given to the 550k patients on dialysis in the US?
Three times a week, 12 hrs a week: surely we can work on the setting and the use of time? How about some better chairs, lower light, privacy if wanted, and more sense of community if desired?
Kidney warriors are strong and determined, but we need education about diet, exercise and importantly, ways to get on the transplant list. We also need connections with others.
I hope I can contribute something valuable to the kidney community after spending these weeks in April on dialysis. I pledge to keep trying!
Continue reading part 3 of Karin’s journey: Day of Transplant Surgery


Today I received my new kidney, lovingly called, Croissant – Lisa.
My sister and I were driven to the hospital at 4:30am by our parents, Ulla and Michael. We were a strong team, and my father reminded us of the many trips the four of us had taken when Lisa and I were children. Conversation on the way into NY Presbyterian was light and the sun kept rising while we were approaching the huge complex of medical buildings.
Wearing blue paper masks, we all marched into the heart center which is where you register and wait together. My head leaned on Lisa’s shoulder when they first called her name, and she walked in bravely, together with our father. A few minutes later they called my name, and my mother and I followed.
Now followed hours of waiting with questions, IV placements, blood draws and consent signatures to get us ready for surgery that was going to take place at 8am for Lisa and three hours later for me. One of her kidneys was going to be removed and placed into my right iliac fossa (lower right abdomen/pelvis). Our surgeons were confident. Mine walked in stylishly outfitted in a suit and dress shoes, and I asked “Aren’t you dressed yet?” He answered, “I am dressed – PJs come on shortly.”
Before Lisa was given her sleeping potion, I had the opportunity to see her on the OR table and it brought tears to my eyes. Of course I had thought extensively about her gift to me, but never this concretely – this was tangible, palpable even. My little sister Lisa is going under, and being cut open, for me to survive.
She is my hero for life. She has always been extremely loyal and stubborn. She doesn’t give up and she loves big. I know that about her, and I also know she fights hard and pushes through pain. As she was lying on that table, she was beautiful. I wish I had taken a picture. She looked serene, even happy.
Back in my cubby, my mother and I kept waiting for my turn. I slept a little, and we talked a little. It was a nice way of waiting, and I appreciated my mother’s way of distracting me yet leaving me alone when I drowsed off.
When I was rolled toward the OR, my tears started again. I thought of Liv, my family and my life. I know the likelihood of mortality in these procedures is extremely low, but any surgery poses a risk. I don’t think it was that risk that made me teary-eyed though. It was the magnitude of the event and the many consequences that were all playing out in my head that caused the tears to flow: pain, graft failure, nausea, long hospital stay, cold OR, etc, etc.
On the table a few minutes later, I was treated so well by the nurses and anesthesiologists, who all addressed me as Dr. Hehenberger and gave me both respect and empathy. The Benadryl I had been given earlier, combined with the fentanyl they now infused, put me out almost immediately. It was many hours later when I woke up in the recovery ward with a kidney that already had excreted urine on the OR table! Croissant – Lisa had come alive inside my body, and I was delirious with joy.
I wanted to hug and kiss the world, and the doctors who came by all received my affections. Since I was lying down, I kept reaching for hands to hold and faces to smile at. My mask restricted me, but perhaps it was good to not show such a clownish smile to the world.
I am now facing four days of chemo light (thymoglobulin) and steroids as the induction therapy, while also getting my regular immune suppressants to make sure Croissant – Lisa doesn’t get rejected by my immune system. That is going to involve some side effects, such as higher blood sugars etc, but I am hoping I can keep that initial smile in my mind and push through the acute pain to eventually yield my goals, which near-term are to go home, kiss my daughter, hug my parents and other sister Anna, and toast Lisa – my hero.
Continue reading part 4 of Karin’s journey: The Gift


How do you thank someone who gave up a piece of themselves for you? How do you express gratitude for feeling alive again after a period of suffering enormous fatigue, nausea, fear and depression?
My sister and my father did this for me – they each gave up a kidney to save my life.
14 years ago, my father and I were on the table, and these fourteen years have enabled me not only to smile and hug my family and friends, but also to have a child of my own and start and build a thriving life sciences company that serves patients and promotes innovation.
This past week, my younger sister Lisa did the same for me. Her kidney came alive in my body immediately on the OR table and normalized my kidney values within two days of the operation. It is hard to describe my feelings and my energy levels other than as “hyper”.
I want to run, laugh, hug, scream and jump for joy. I want to bring joy to others, smiling to every person I meet, including the incredible staff at Columbia Presbyterian, led by the amazing Dr. Lloyd Ratner. He has assembled a team of surgeons, physicians, scientists, nurses, physician assistants (PA), technologists, social workers, occupational therapists, and other staff who work tirelessly under very hard conditions. They are heroes, together with the donors who give us recipients a second (or third) chance of life.
So what am I going to do with this gift?
I will live every day to the fullest, which doesn’t mean I will do as much as I can every day, but I will measure myself and take care of my new “baby” so that it can serve me as long as possible.
I will take care of my body by eating right, sleeping enough, exercising regularly and practicing mental health through meditation and mindfulness. I will be kind to myself when I feel tired, and I will be respectful to others and always keep in mind that the exterior of someone is not always a reflection of their inner self. I will cherish my friends who have stood by me through the hardship of kidney failure and dialysis.
I will continue to serve patients through my work. I will partner with great companies and leaders in academia to promote innovation. I will provide opportunities for my team to both grow professionally while also taking care of their families.
Above all, my life is dedicated to the family who saved me, and my own little family, whom I am raising with all of my heart. I appreciate each of my sisters, parents, brothers in law, nieces and nephews, and especially my daughter.
To my daughter, I want to show that life may not be a walk in the park – you need to fight for what you want – but it is beautiful. I want her to know that she will always be taken care of, and endlessly loved by, her Mamma.
Continue reading part 5 of Karin’s journey: Going Home

Going home from the hospital was, in many ways, the best experience, but it was also a scary one.
I got to hold my daughter, sleep in my bed, take a shower and eat what and when I wanted to.
However, the protective nature of the hospital and its personnel was lost, and it scared me a little.
Those wonderful nurses, the long line of doctors rounding each morning, even the food cart with its very mediocre yet nutritious food that was given to me on a tray. Do I actually miss this?
Now everything was up to me.
Taking my pills at the right time, measuring my weight and blood pressure daily, making my bed, and being social in a way I had not needed before.
All this took energy. Frankly, it gave me a little fear.
It is interesting since I am, in many ways, a control freak. I crave being in charge of my own actions and outcomes. Yet in four short days I had forfeited that responsibility and surrendered to the hospital.
It took me a full day, but on Day 6, which is Day 2 at home, I feel more myself again. Now I am already longing to drive myself, to be “back” fully.
My promise remains true, to myself and to my family, to take it slow. So my energy is going to be expended toward walks, conversations with my sister, story time with my daughter, and planning for a beautiful garden this spring!



My name is Michael Hehenberger and I donated a kidney to my daughter Karin in March, 2009. I was borderline “old” because I was 63 years old and they usually have an age limit of 60, but I was accepted after going through a lot of tests. They don’t want to do an expensive procedure with two operations going on in parallel where the end result is not acceptable, as they don’t want to waste those resources. They generally feel a 63-year-old kidney may not be as good as a younger one, but so far so good.
I decided to be a donor when my daughter told me that her kidneys were close to not working anymore. She had diabetes and her kidneys suffered, as well as her eyes, and she was approaching kidney failure. When I heard that, she didn’t have to ask me the question. I told her that I would donate a kidney to her.

My biggest fear before donating was that they would take the kidney and put it into my daughter’s body, and then it wouldn’t work. I was never nervous about the actual surgery or the recovery afterwards.
I was first tested for genetic compatibility, and I passed that test. As a father, it’s not automatic that you can be a donor; the best donors are siblings because brothers and sisters are more similar genetically. Once I passed the genetic test, I then had to go through all kinds of fitness tests to make sure both that my kidney was healthy enough for my daughter and that I was healthy enough to go through the operation.
I was very well informed before being a donor and was provided with all of the information I needed. I developed a very good relationship with my surgeon; he’s a great person. I was running and working out to prepare for the operation, so I was in really good shape. There are lots of statistics that donors live as long as non-donors, but I think it’s difficult to compare because the donor population is, on average, healthier than the rest. In order to be a donor, you need to be on the upper end of the spectrum when it comes to health and fitness.
For me, the recovery process was extremely quick. I didn’t take any strong pain medicine, just some Tylenol. It was really easy, and I got back to normal very quickly. I started running again after two weeks. I had three post-op appointments with my surgeon to make sure everything healed properly. I’m also getting regular blood tests every year and they are measuring my renal parameters, so I’m getting very good care.
I have not experienced any difference in my life after donating; I can eat and drink and do everything the same as before. I had the operation in March, and in May I did quite a strenuous hike at the foothills of the Himalayan mountains. I had planned it with friends prior to deciding to be a donor, and I really didn’t want to miss it. I was able to come back and after less than two months, I was able to participate and do the five-day hike.
Being a donor has motivated me to stay healthy and take care of my remaining kidney. When you do something like donating, you feel good about yourself and you are motivated to come back quickly. I am in a good mood most of the time, and working out is the best way to stay in a good mood.
Looking back, I would absolutely do it again. As I mentioned earlier, my daughter didn’t need to ask me, I told her I would do it. I knew it was necessary, and in that situation, I was the best option. I thought that if I do it now, if or when she needs another kidney, she has two sisters who can potentially donate.
I would tell someone considering being a living kidney donor to not be afraid of living with one kidney; many people live with one kidney and it works; it’s actually quite common. You go through a lot of different, comprehensive, extensive tests and they have a meeting with many doctors to determine if you can safely be a donor. It’s not just one person making the decision. I’m still alive after 10 years, and still feel really good about my decision to donate.
